Breast Implants 101: A Primer for What you Need to Know
Breast implants and breast augmentation are the bread and butter of Plastic Surgery as breast augmentation has been the top cosmetic surgical procedure in the nation since 2006. When a patient comes in for consultation and the plan reveals itself to be 'straightforward’ breast augmentation (let's face it, is there really anything completely straightforward?), the decisions regarding how exactly to proceed are relatively easy for me to reconcile but I feel strongly that knowledge is power and spend an inordinate amount of time explaining to my patients the pros and cons of every decision made to come to the best conclusion for them. Let me share with you some of these points to perhaps educate yourself if this is something you are considering or perhaps already have breast implants for cosmetic or reconstructive reasons and have some questions.
Silicone or saline?
In 2019, 85% of breast implants placed in the United States were silicone gels and 15% were saline. This reflects decisions in my practice as well. Silicone implants are very safe and look and feel very natural but these implants carry with them the need for implant surveillance (MRI or high-resolution ultrasound) as the cohesive nature of the gel prevents the structure from losing volume and shape if ruptured. Saline implants do not require surveillance because when they rupture, they deflate-which means your body absorbs the saline they are filled with. Saline implants tend to exhibit more rippling which can be visible or just identified by feeling the implant. Silicone implants carry a higher rate of capsular contracture or excessive scar tissue around the implant that may result in the breast becoming progressively hard or misshapen, than saline implants.
(Learn more about the types of breast implants offered at our office by clicking the following links: Allergan, Mentor, Sientra.)
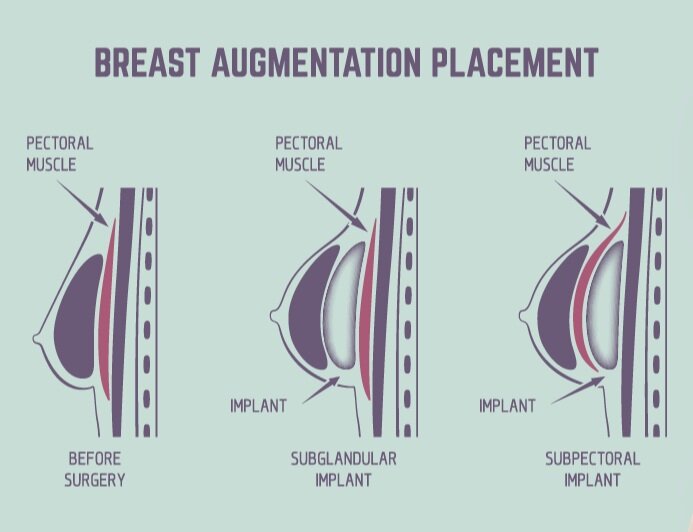
Over or under 'the muscle'?
'The muscle' is how most patients refer to the pectoralis major, the muscle on the chest wall that defines the plane the implant will be placed in. As with every other decision, there are pros and cons to placing the implants over or under the muscle. This muscle runs from the top of the long bone in the upper arm to the breastbone; it is a thin muscle that can help cover the upper part of the implant in a very thin patient. My decision to place an implant under the muscle is strictly based on how thin the patient's tissues are in the upper pole of the breast. If adequate natural tissue is present (tissue pinch at or above 3-4 centimeters), I prefer the implant placed over the muscle for a more natural appearance and avoidance of draping the muscle over the implant which can lead to animation deformity or movement of the implant when the muscle is flexed. Because of the massaging action of the muscle in everyday activity, capsular contracture rates are lower in this plane than over the muscle. If the tissue coverage allows implant placement over the muscle, this results in a very natural appearance and feel of the breast without animation but this plane carries a higher risk of capsular contracture. As I tell all of my patients, there are not any perfect decisions when breast implants are discussed.
What is capsular contracture?
When an implant is placed in the breast-over or under the muscle, cosmetic or reconstructive, silicone or saline- the body's natural response is to create scar tissue around the device. This is important as a capsule (the natural scar tissue) helps to anchor the implant where it is placed at the time of surgery and is a necessary step in recovery from the procedure. Capsular contracture is too much scar tissue and the effects may be very subtle (class I-no breast firmness or pain, class II-firm but no pain) or more significant which may require surgical intervention(class III-breast firm and distorted without pain, class IV- firm and distorted with pain). There are many theories regarding why this occurs and many protocols during surgery proven to minimize the risk but it still occurs. It is more common in silicone implants than saline implants, both when placed over and under the muscle.
Is there a timeline for replacing my breast implants?
If it ain't broke, don't fix it. Many patients believe that they will have to have their implants replaced at the 10-year anniversary of their surgery. This is not true in the absence of any concerns about the implants. Saline breast implants have a 10-year warranty; if you experience rupture prior to this time, you can get assistance toward replacing that implant. If you reach the 1o year timeline and they look great, leave them alone. If you are happy with your implants, you do not have pain or distortion of the breasts from capsular contracture and surveillance has confirmed your silicone implants to be intact (current protocol from the FDA is an MRI at 3 years after implantation then every 2 years), leave them alone. The warranty for silicone implants varies with the manufacturer (Allergan: lifetime replacement if ruptured, advanced capsular contracture warranty for replacement for 10 years; Sientra: lifetime replacement if ruptured, advanced capsular contracture warranty for replacement for 20 years; Mentor-lifetime replacement if ruptured, advanced capsular contracture warranty for replacement for 10 years.)
(Click the link to read more about implant warranties for Allergan, Sientra, or Mentor implants.)
What is Breast Implant Illness?
Breast implant illness or BII is a wide spectrum of vague symptoms over the entire body that is thought to originate from the existence of breast implants, both silicone and saline. Symptoms can include joint and muscle pain, chronic fatigue, sleep disturbance, rashes or skin problems, anxiety, depression, GI problems, and a long list of additional symptoms. The origin of these symptoms is thought to be autoimmune or inflammatory-related but the challenge is proving that the implants are indeed the source prior to removal of them. Most patients have exhausted other sources of these symptoms in concert with their primary care physician or GYN or another specialty physician (Rheumatologist or Endocrinologist) and elect to have the breast implants removed as a final step in attempting to alleviate these concerns. If a patient is considering the removal of breast implants in an attempt to relieve some of these symptoms, it is very important to note that no surgeon can guarantee resolution of systemic symptoms after implant removal although many patients do report they slowly feel better with time. It is important to discuss the aesthetic appearance of the breasts after implant removal, especially in thinner patients with less natural breast tissue. The breast can appear very deflated and, after removal of the capsule around the implant as part of the procedure, scarred to the chest wall. This scarring softens with time and many patients are satisfied with the results. Patients need to be aware that if they had breast implants removed with concern for BII and symptoms did not resolve after implant removal and the patient was dissatisfied with the appearance of their breasts, they could have implants replaced at a later time.
What is ALCL?
Anaplastic large cell lymphoma, or specific to our specialty Breast Implant-Associated ALCL (BIA-ALCL) is a rare type of lymphoma related to textured devices, tissue expanders, and breast implants, used for cosmetic and reconstructive surgeries. As of July 2019, there were 573 cases worldwide and 33 deaths. Textured devices are the common denominator in the development of this disease and to date, it has never been diagnosed in a patient with a history of exclusively smooth devices. It is known to develop on average 8-10 years after placement of the implant and may present as pain, a mass, swelling, or a fluid collection in the breast around the implant. Treatment after a thorough evaluation is surgical with the removal of the capsule around the implant (where the malignancy is present) and the implant itself. If a patient has no evidence of disease elsewhere, no other treatment is indicated and a patient could consider implant replacement at a later time if desired. There have been locally advanced cases at diagnosis that required chemotherapy and/or radiation and metastatic cases that resulted in death. This is a rare disease and there are specific protocols to evaluate and treat suspected BIA-ALCL. Knowledge of this disease should not be a deterrent if considering breast augmentation.
What do I do if I have textured implants now? Should I have them removed?
The FDA has stated that a patient with a textured device in the absence of any concern for their implants and without suspicion of BIA-ALCL does not have to proceed with implant removal. A certain manufacturer was directed by the FDA to voluntarily recall a series of their textured devices and this caused anxiety with those patients with the recalled implants. If you have textured implants or are not sure whether or not you do, it would be smart to contact your Plastic Surgeon to discuss options and, if any concerning signs are present in your physician's opinion, proceed with evaluation and treatment.
How long will my implants last?
Good question. No one knows. There is not a forever breast implant: any patient considering breast augmentation must be prepared for additional surgeries in the future. Most surgeons would predict 10 to 15 or even 20 years or more prior to any implant revision in the absence of significant changes in body weight and natural breast tissue and with implant surveillance for silicone gel implants indicating that they are intact...but there will be additional procedures if an implant is placed. I see my breast implant patients, both silicone gels and saline, once a year forever. At that annual visit, we discuss changes in the breast, the timing of surveillance if indicated, and the patient's satisfaction with the appearance of their breasts. If all is well and all boxes are checked off, we follow up one year later and repeat the same questions. At any time if a patient has any concerns for their breasts, they are brought back to the office for a bonus check to determine what is going on and move forward from there.
By now you can see that there are as many questions as answers when it comes to breast implants. I had breast cancer four years ago and during my reconstructive journey, I have had both textured and smooth implants and had them both under and over the muscle. I can talk to you about breast implants, as both a surgeon and a patient. For a patient considering this for cosmetic reasons or facing reconstruction of the breasts, this information is essential for baseline education. For patients with implants in place for any period of time-silicone or saline, textured or smooth...or maybe not known-this primer may be the motivation to make an appointment to size up the situation and gain some knowledge about something that concerns you or just for peace of mind. Knowledge is power. Power is sexy. Be powerful, safe, and sexy and get smart about your implants.